A Bidirectional Relationship: Exploring the Interplay Between Asthma and Anxiety
- Sep 30, 2025
- 7 min read
Olivia Mickles

We cannot always control how our bodies function, but we can learn to control how we mentally deal with the ailments we may face. Some studies suggest that our mentality alone is enough to drastically alter our physical state, worsening existing conditions such as panic attacks, hair loss, and autoimmune diseases. This article will focus on how anxiety can exacerbate chronic asthma, and vice versa, and how affected individuals can learn to manage their anxiety to improve long-term well-being.
How does anxiety affect our brain and body?
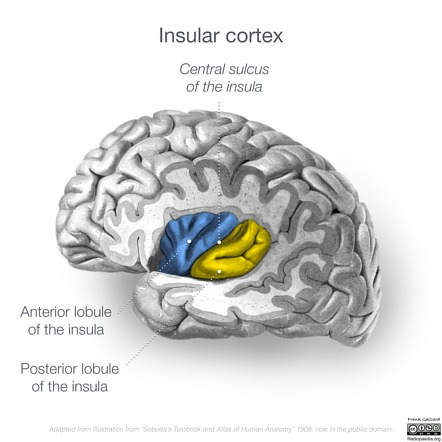
Stress and anxiety do far more to the brain and body than simply making us feel worried, overstimulated, or worn out. Prolonged exposure to stress can lead to heart disease, high blood pressure, weakened immunity, sleep disturbances and many other ailments that diminish quality of life. High anxiety amplifies activity in the anterior insula, mid-insula, and perigenual anterior cingulate regions of the brain, which are involved in the processing of emotions, sensory information, and regulating autonomic nervous system responses. Disruption in these areas can reactivate microglia and astrocytes, glial cells that support neurons and maintain brain function in the medial prefrontal cortex and amygdala.

The amygdala is a primary center for emotion processing, particularly fear, in the brain. Research has shown a negative correlation between anxiety and amygdala volume, meaning as anxiety increases the volume of the amygdala decreases. Anxiety is also linked to chronic inflammation that alters the structure of white and gray matter of the brain, leading to further volume changes (Dehdar & Raofy, 2023). These structural deformities can lead to overactivation of the amygdala, heightening fear, fueling chronic anxiety, and disrupting both mental processes and physical functioning.
What is asthma?

Asthma is a chronic lung disease that, according to the World Health Organization (2019), affects around 262 million people worldwide and caused about 455,000 deaths in that year alone. It can develop at any age, sometimes present at birth and in other cases triggered later by smoking, pollution, obesity, or other medical conditions. Asthma occurs when the airways become hyperresponsive, inflamed, and tighten the muscle around the airways, making it harder to breathe. Symptoms range from mild to severe, including coughing, wheezing, shortness of breath, and chest tightness. Unsurprisingly, such symptoms often heighten stress and anxiety about health (World Health Organization, 2024).
No matter if you have milder allergic asthma or severe chronic asthma, treatment usually involves inhaled corticosteroids to manage symptoms, helping patients maintain a normal life. Beyond staying on top of taking medication, managing asthma requires knowing and avoiding personal triggers as much as possible.
Anxiety-related neurobiological modifications in those with allergic asthma
Allergic asthma, though less life-threatening than severe asthma, is still a risk to an individual's well being, health, and mental state. Allergic asthma activates IgE, a type of protein that plays a key role in allergic reactions, that causes inflammation in brain areas linked to anxiety, similar to the inflammation anxiety itself can trigger in the amygdala and prefrontal cortex. Together, allergic asthma and anxiety may intensify anxious feelings and alter brain volume. It suggests a possible immune-brain communication mechanism being the reason for the inflammatory responses in specific brain areas for asthma patients with psychiatric disorders (Dehdar & Raofy, 2023).
Animal studies support these findings. A rodent study showed that rats exposed to allergens had more intense anxiety-like behaviors. The allergens increased TH2 cytokines and corticotropin-releasing factor, which play a crucial role in immune response, in the prefrontal cortex, triggering the release of adrenocorticotropic hormone and glucocorticoids, key regulators of stress and emotions. (Tonelli et al., 2009) These findings suggest allergens can worsen anxiety by disrupting natural stress regulation, explaining why breathing issues often accompany anxiety and allergies.
Neuroimaging research also reinforces this link. An MRI study of allergic asthma patients revealed smaller hippocampal volumes than healthy control subjects, most likely due to structural alterations caused by inflammation and high stress from a young age (Carlson et al., 2017). Since the hippocampus is our center for memory and learning, structural alterations can lead to functional problems such as memory loss, difficulty making decisions, and the inability to regulate the HPA axis. If the HPA axis is unregulated, hormones responsible for responding to stress can become hyperactive and increase our feelings of anxiety. This is yet another piece of evidence that supports the theory that brain inflammation can cause cognitive decline in asthmatics and anxiety patients, as well as the existence of a possible immune-brain communication mechanism being responsible for it all.
How anxiety affects health related quality of life within the context of asthma
Many people strive to maximize their quality of life, yet mental or medical conditions, or even both, can make this far more challenging to accomplish. A recent study showed that individuals with severe asthma had worse mental and physical health related quality of life (HRQoL) with corresponding higher anxiety and depression scores than individuals without asthma. Severe asthma patients also expressed stronger beliefs about the essential nature of their medication than those without the condition. They also reported having high anxiety over accessibility to medication as well as its side effects. As corticosteroids are required by all chronic asthmatics to be able to breathe daily, it is something they could literally not go a day without; yet taking corticosteroids daily, especially from young, can have mild to moderate side effects. It would therefore be beneficial to integrate psychological techniques to reduce anxiety and lower concerns in regards to managing the disease and treatment. This addition could also avoid the problem of poor adherence to treatment, caused by high anxiety and subsequent suspicion, which could in turn further damage an individual's quality of life. (Rönnebjerg et al., 2023)
Why is taking mental HRQoL seriously in individuals with chronic diseases like asthma so important? High mental HRQoL is positively correlated with high self-efficacy, or the belief in one’s own ability to thrive in accomplishing goals and navigating difficult situations. Common symptoms in anxiety and depressive disorders include feeling hopeless, worthless, scared, alone, and experiencing anhedonia, the general reduction of feelings of enjoyment or pleasure from activities that promoted those feelings in the past. Symptoms like these can cause individuals to become isolated, take part in substance abuse or self harm, medical neglect, and a wide range of other destructive behaviors. By addressing this “dark side” of the disease, doctors can not only treat patients with corticosteroids, but also with anxiety reducing and calm inducing methods. Research has shown that high mental HRQoL was also negatively correlated with anxiety, meaning that those with more positive mentalities had a decreased likelihood of experiencing anxiety, depression, or other related disorders. (Rönnebjerg et al., 2023)
Why does this matter?
Studying the correlation between asthma and anxiety can lead to new discoveries focused on improving the lives of millions of people worldwide. This potential new information could also shed light on the interaction of mental disorders with other chronic diseases as well. By becoming more educated on this topic, doctors and researchers may be able to find new ways to care for patients that improve their mental quality of life alongside caring for their physical health.
Could we create a new medication that controls airway inflammation and lowers anxiety? Is there a way to help reduce brain inflammation caused by asthma, anxiety, and allergies to reduce the risk of volume changes and negative cognitive impacts? Maybe we could, but we have to keep researching in order to find it.
Future research should aim to seek understanding in the gray areas of the research on this topic. A gap in the literature can be seen in certain inconsistent findings such as how women show significantly more symptoms of anxiety than men and generally have a worse mental health quality of life; yet, there are no significant differences in mental HRQoL between the sexes. Why is this? Moreover, there was no significant physical health quality of life difference between the genders and it is currently unknown why women may have a greater mental struggle in general. Another interesting question for future research could focus on the difference between individuals who have had “a life before asthma” versus those who “never knew a life without asthma” (Rönnebjerg et al., 2023). Would the ratings of quality of life be higher for those who developed the disease early in life because they do not know the difference of being non-asthmatic, or would HRQoL be lower because they have never known a life without the struggles of the disease? A child would react to a diagnosis as severe as asthma much differently than an adult who may already have some knowledge about it, so it is important to modify how different patients are treated by the professionals taking care of them.
Exposure based cognitive behavioral therapy (CBT) for anxiety has been hypothesized to be a good starting direction for those experiencing anxiety. In an individual with chronic asthma, the risk of developing an anxiety disorder is doubled than for non-asthmatics. So, why not make CBT part of the treatment regimen? One can start by acknowledging their negative thoughts and reframing them to be less intimidating, facing fears, and finding new ways to work on problems to make them feel more manageable. Anxiety can lead to hypervigilance over a disease such as asthma, which is helpful in moderation but can easily turn into excessive fear and avoidance. Recognizing this issue is key for future treatment. A study of the effectiveness of this kind of treatment resulted in all participants, by the end, at least somewhat improving (to different extents) their control over their asthma and anxiety symptoms (Bonnert et al., 2020). By fine tuning symptom management strategies for both conditions, asthmatics can learn through therapy how to handle generalized stress and how to stop catastrophizing about their symptoms.
References
Bonnert, M., Andersson, E., Serlachius, E., Manninen, I., Bergström, S., & Almqvist, C. (2020). Exposure‐based cognitive behavior therapy for anxiety related to asthma: A feasibility study with multivariate baseline design. Scandinavian Journal of Psychology, 61(6), 827–834. https://doi.org/10.1111/sjop.12674
Carlson, S. M., Kim, J., Khan, D. A., King, K. S., Lucarelli, R. T., McColl, R. W., Peshock, R. M., & E. Sherwood Brown. (2016b). Hippocampal volume in patients with asthma: Results from the Dallas Heart Study. Journal of Asthma, 54(1), 9–16. https://doi.org/10.1080/02770903.2016.1186174
EZProxy AFX Authentication Page. (2025). Lehigh.edu. https://www-sciencedirect-com.ezproxy.lib.lehigh.edu/science/article/pii/S0361923023001521?via%3Dihub
Rönnebjerg, L., Axelsson, M., Hannu Kankaanranta, & Ekerljung, L. (2023b). Health-related quality of life, anxiety, depression, beliefs of medication and self-efficacy in individuals with severe asthma – a population-based study. Journal of Asthma, 1–12. https://doi.org/10.1080/02770903.2023.2248512
Tonelli, L. H., Katz, M., Kovacsics, C. E., Gould, T. D., Joppy, B., Hoshino, A., Hoffman, G., Komarow, H., & Postolache, T. T. (2009). Allergic rhinitis induces anxiety-like behavior and altered social interaction in rodents. Brain, Behavior, and Immunity, 23(6), 784–793. https://doi.org/10.1016/j.bbi.2009.02.017
World Health Organization. (2024). Asthma. World Health Organization; World Health Organization. https://www.who.int/news-room/fact-sheets/detail/asthma




Comments