Embodiment in Action: Applications for Rehabilitation
- Jul 8, 2025
- 7 min read
Catherine Gooch
Background
The experience of having a physical self, of understanding our bodies as our own and as being contained within certain physical boundaries, is something so automatic that we tend to not even consciously notice it. But this sense of embodiment can unfortunately become damaged by certain injuries. Because of this, researchers have been exploring embodiment as a clinically-useful outcome in various types of rehabilitation research.
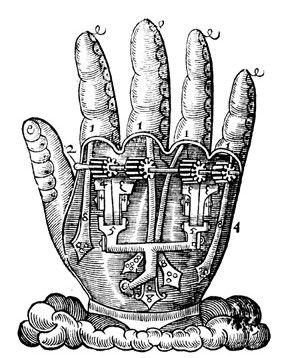
To better understand this, it will be helpful to have a clearer framework for what exactly embodiment is. One useful model consists of three main components: ownership, body representation, and agency (Segil et al., 2022) (Figure 1). Ownership is the belief or feeling that a limb, tool, or device is a part of yourself, rather than some external object. Body representation refers to “the knowledge, beliefs, and experiences we have of the physical structure of our bodies” (5). This includes things like knowing the size or location of our bodies, as well as understanding the boundaries of our bodies and which objects are close enough to be acted upon by us. Lastly, agency has to do with the self-attribution of our actions, or the feeling that we are in control of the movements we make. All three of these components can be experienced either consciously or subconsciously and are phenomenologically separable, meaning the subjective experience of one can occur without the subjective experiences of the other two. However, the processes that underlie each domain also play a role in the others, meaning they “are not separable on the level of neurophysiological mechanisms” (3).

Applications
This concept has relevance to fields such as prosthetics. It has been shown that prosthetic devices can become integrated into an individual’s perception of their own body (Marasco et al., 2011, Fritsch et al., 2021, Page et al., 2018). One interesting way of measuring this is by using the skin conductance response, which is the change in electrical conductivity of a person’s skin as they release sweat in response to some type of arousal. In one study, researchers used this response to investigate embodiment of a prosthetic hand after the participants experienced a version of the famous ‘rubber hand illusion’ (Ehrsson et al., 2008). The experiment was set up so that the participants’ stump was covered, and a realistic, rubber prosthetic hand was placed in full view in front of them. The researchers elicited a fear response by stabbing both the stump and the rubber hand with a needle attached to a syringe. While this was happening, they measured skin conductivity with electrodes placed over the area of the stump where the participants’ fingers would have been. This was performed in two conditions: one where the stump and the prosthesis were stabbed at precisely the same time, and one where they alternated. Interestingly, the researchers observed a greater skin conductance response in the synchronous condition compared to the asynchronous condition. This indicates that the participants experienced a greater sense of subconscious ownership of the prosthesis when it was stabbed at the same time as their stump. Further, it shows that embodiment, and particularly embodiment of external devices such as a prosthesis, is not static – rather it can be increased or decreased in response to external stimuli.
Because embodiment can be modulated like this, researchers can design rehabilitation programs to promote this sense, and use it to improve recovery after certain injuries. One study took an embodiment-based approach to improve orthopedic rehabilitation in patients with distal radius fracture (Matamala-Gomez et al., 2022). In this study, researchers split the participants into three groups: an immersive virtual reality (VR) experimental group, a non-immersive VR control group, and another control group that performed conventional rehabilitation exercises focused on moving their hand and fingers. Patients in the immersive VR group wore a headset that displayed a virtual body through a first-person perspective, and performed a variety of tasks where they pressed a pedal to move their virtual arm while receiving tactile feedback on their immobilized real arm. Patients in the non-immersive VR group only observed virtual actions, rather than performing them by pressing the pedal; they also did not receive any sensory feedback. Participants in each group performed their exercises for 4-6 weeks after their arm was put in a cast, and then performed the same conventional rehabilitation exercises for 6 more weeks after their cast was removed. Participants in the immersive VR group had the greatest recovery in functional ability of their arm, as well as range of motion in their wrist. Additionally, results from an embodiment questionnaire showed that participants in the immersive VR group had stronger feelings of both ownership and agency of the virtual limb compared to participants in the non-immersive VR group. Importantly, there was a strong positive correlation between embodiment scores on the questionnaire and functional recovery of the participants’ arm after their cast was removed. The researchers suggest that “the feeling of ownership toward a virtual body may increase sensorimotor activation when the embodied virtual body performs movements over which the subject has a sense of agency,” which could be a reason for the improved motor function in the immersive VR group. Overall, this study shows the potential for utilizing embodiment-based approaches in rehabilitation.
Another application of embodiment for rehabilitation is in robotic exoskeletons. These are a type of assistive device which can provide support for functions such as walking. There are a few different robotic exoskeletons currently available on the market, but their full potential for improving muscle function is not yet known. One newly-developed robotic exoskeleton was built by researchers to assist people with hemiparesis, or muscle weakness on one side of the body after stroke, in walking (Lora-Millan, J.S., et al., 2022). The researchers specifically examined how the exoskeleton was embodied by the users after gait training (Figure 2). This is important to examine, because the maximum benefit of these devices can only be achieved when they “are embodied by users, i.e. the wearer considers that the device’s action is performed by their own body rather than by an external tool” (Lora-Millan, J.S., et al., 2023).

The researchers did this by looking at the changes in muscle activity of the wearers (Lora-Millan, J.S., et al., 2023). The idea is that as the exoskeleton becomes embodied by the user, their muscle activation patterns will change to reflect that. In particular, the researchers expected to see reduced muscle activity in the non-paretic leg as the participants develop greater senses of agency over the device, incorporating it into their body schema and reducing energy expenditure while walking. These results have been found in other studies that use robotic exoskeletons, but mostly with healthy subjects (Haufe et al., 2021, Wehbi et al., 2017, Steele et al., 2017, Gordon & Ferris, 2007). In this particular study, though, the researchers found mixed results, with some participants demonstrating these characteristics of embodiment and others not, which they attribute to the wide variety in time after stroke and degree of impairment among the study participants, as well as potentially not enough time actually using the device. Overall, these results emphasize the need to better understand how the nervous system’s ability to embody external devices is impacted by stroke, and how this crucial function can be restored to improve rehabilitation outcomes for stroke survivors.
Future Directions
Embodiment has been shown to be a clinically-relevant outcome in wide-ranging areas of rehabilitation research, from prosthetic devices to virtual reality to robotic exoskeletons and more. However, there are still many questions currently unanswered about how best to foster this in people with neurological or musculoskeletal injuries. Future research should aim to clarify the neurophysiological mechanisms that enable embodiment across different populations and injury types, as well as to standardize measures of embodiment used in research. By doing so, scientists, clinicians, and engineers can work to build improved technologies that restore not only motor function, but a more complete and intuitive sense of self for individuals recovering from injury.
Works Cited
1. Segil, J. L., Roldan, L. M., & Graczyk, E. L. (2022). Measuring embodiment: A review of methods for prosthetic devices. Frontiers in neurorobotics, 16, 902162. https://doi.org/10.3389/fnbot.2022.902162
2. Paul D. Marasco, Keehoon Kim, James Edward Colgate, Michael A. Peshkin, Todd A. Kuiken, Robotic touch shifts perception of embodiment to a prosthesis in targeted reinnervation amputees, Brain, Volume 134, Issue 3, March 2011, Pages 747–758, https://doi.org/10.1093/brain/awq361
3. Fritsch, A., Lenggenhager, B., and Bekrater-Bodmann, R. (2021). Prosthesis embodiment and attenuation of prosthetic touch in upper limb amputees - a proofof-concept study. Conscious. Cogn. 88, 103073. https://doi.org/10.1016/j.concog.2020.103073
4. Page, M. D., George, J. A., Kluger, D. T., Duncan, C., Wendelken, S., Davis, T., et al. (2018). Motor control and sensory feedback enhance prosthesis embodiment and reduce phantom pain after long-term hand amputation. Front. Hum. Neurosci. 12, 352. https://doi.org/10.3389/fnhum.2018.00352
5. H. Henrik Ehrsson, Birgitta Rosén, Anita Stockselius, Christina Ragnö, Peter Köhler, Göran Lundborg, Upper limb amputees can be induced to experience a rubber hand as their own, Brain, Volume 131, Issue 12, December 2008, Pages 3443–3452, https://doi.org/10.1093/brain/awn297
6. Matamala-Gomez, M., Slater, M. & Sanchez-Vives, M.V. Impact of virtual embodiment and exercises on functional ability and range of motion in orthopedic rehabilitation. Sci Rep 12, 5046 (2022). https://doi.org/10.1038/s41598-022-08917-3
7. Lora-Millan, J.S., Sanchez-Cuesta, F.J., Romero, J.P. et al. A unilateral robotic knee exoskeleton to assess the role of natural gait assistance in hemiparetic patients. J NeuroEngineering Rehabil 19, 109 (2022). https://doi.org/10.1186/s12984-022-01088-2
8. Lora-Millan, J.S., Sanchez-Cuesta, F.J., Romero, J.P. et al. Robotic exoskeleton embodiment in post-stroke hemiparetic patients: an experimental study about the integration of the assistance provided by the REFLEX knee exoskeleton. Sci Rep 13, 22908 (2023). https://doi.org/10.1038/s41598-023-50387-8
9. Haufe, F.L., Kober, A.M., Wolf, P. et al. Learning to walk with a wearable robot in 880 simple steps: a pilot study on motor adaptation. J NeuroEngineering Rehabil 18, 157 (2021). https://doi.org/10.1186/s12984-021-00946-9
10. Wehbi, F. et al. Active impedance control of a knee-joint orthosis during swing phase. In 2017 International Conference on Rehabilitation Robotics (ICORR) 435–440 (IEEE, 2017). https://doi.org/10.1109/ICORR.2017.8009286.
11. Steele, K. M., Jackson, R. W., Shuman, B. R., & Collins, S. H. (2017). Muscle recruitment and coordination with an ankle exoskeleton. Journal of biomechanics, 59, 50–58. https://doi.org/10.1016/j.jbiomech.2017.05.010
12. Gordon, K. E., & Ferris, D. P. (2007). Learning to walk with a robotic ankle exoskeleton. Journal of biomechanics, 40(12), 2636–2644. https://doi.org/10.1016/j.jbiomech.2006.12.006




Comments